Efficacy of Behavior Therapy and Parent Management Training in Treating Schizophreniform Disorder
* Nuzhat-ul-Ain
Centre for Clinical Psychology, University of the Punjab, Lahore
Najma Badar
Services Hospital, Lahore
Institute of Applied Psychology, University of the Punjab, Lahore
This case study describes the management of Schizophreniform Disorder in a 16 year old adolescent male, an inpatient at the Psychiatry Department of the Services Hospital, Lahore. The intervention was comprised of different strategies of Behavior Therapy and Parent Management Training. The treatment comprised of 19 sessions with duration of 45 minutes. The treatment was done for over a period of 3 months. The patient was referred to clinical psychologist and accompanied by his mother with the complaints of anger issues, physical aggression towards the mother, stubbornness, abusive language, suspiciousness towards the mother, hiding belongings of other family members and hoarding them in his room, not leave his room for the last 2-3 months, inappropriate association and interaction with a pet cat, poor self-care and medical non-compliance. Assessment was done on the basis of diagnostic criteria in DSM-5 and Brief Psychotic Rating Scale (BPRS). The patient was diagnosed with 295.40 (F20.81) Schizophreniform Disorder without good prognostic features. It was hypothesized that Behavior Therapy would reduce the behavioral complaints (anger, stubbornness, hoarding things, not leaving the room, inappropriate interaction with pet cat, poor self-care and medicine non-adherence). Moreover, Parent Management Training would help in resolving familial issues which could be contributing factors towards the patient‟s illness. ABA research design was employed. In phase-A, psychological assessment was conducted. The current case srudy was conceptualized by Zubin and Spring (1977)
* Correspondance concerning this article should be addressed to Nuzhat-ul- Ain, MS Scholar, Centre for Clinical Psychology, University of the Punjab. Email: nuzhatulain4@gmail.com
Najma Badar, Clinical Psychologist, Services Hospital, Lahore.
Stress Vulnerability Model. During Phase B, the treatment phase, Mr. X was treated by using Behavior Therapy, while his mother was offered Parent Management Training. Comparison of pre and post treatment assessment showed marked decrease in the severity and duration of symptoms of the patient. It concluded that Behavior Therapy and Parent Management Training simultaneously were effective for treatment of the symptoms of schizophreniform disorder.
Keywords: : schizophreniform disorder, behavior therapy, parent management training
Schizophreniform disorder occurs in 0.07% of the population (Perälä et al., 2007). The symptoms of schizophreniform disorder include, delusion, hallucination or disorganized speech, grossly disorganized or catatonic behavior and negative symptoms of psychosis. In developing countries the incidents of schizophreniform are higher than developed nations. About one third of the patients recover within 6 months of the onset of the disorder while the rest receive the diagnosis of schizophrenia (American Psychiatric Association, 2013).
Schizophreniform disorder is a short-term disorder with symptoms persisting from one month to less than six months. There are various factors which contribute towards its onset, include genetics and environmental. Having a family member with the history of schizophrenia or schizophreniform disorder increases the risk of developing schizophreniform disorder (American Psychiatric Association, 2013). Other factors are environmental that include exposure to stressful environment, dysfunctional or broken families, death of loved ones and other life stressors (Leckman, 2000; American Psychiatric Association, 2013).
Schizophreniform disorder affects both men and women. Men aged 18 to 24 are more vulnerable to suffer from schizophreniform, while women are more vulnerable between the age range of 24 to 35. According to DSM-5, two third of individuals suffering from schizophreniform eventually receive the diagnosis of either schizophrenia or schizoaffective disorder (Leckman, 2000; American Psychiatric Association, 2013). Prognosis of schizophreniform disorder depends on genetic factors and the severity of the episode, with a family history of schizophrenia resulting in poor prognosis.
Treatment
Behavior Therapy is an empirically tested and successful treatment of schizophrenia or schizophreniform. Chambless and Ollendick (2001) suggested that as compared to other modalities, Behavior Therapy includes token economy and contingency contracts are most effective methods to deal with the behavioral complaints of patent with schizophrenia, especially with children and adolescents. It is effective especially in order to reduce odd behaviors and improve self-care and hygiene of the patient because at initial level patients need to improve health related behaviors issues (Chan, 2017; Liberman & Kopelowics, 1995; Thyer, Irvin, & Santa, 1984; Trygstad et al., 2002).
Parent Management Training is important for the management of early onset of psychosis (Agee, Spezze, & Underwood, 2014). It is not only useful in improving the parents‟ understanding by educating them about the illness of the patient (psychoeducation) and its onset and phases (prodromal, onset and residual) but also assists them how to deal with it. If parents are able to recognize the early warning signs and symptoms, they might be able to manage the illness before the person reaches the diagnosis of schizophrenia (Agee, Spezze, & Underwood, 2014). Parent Management Training helps and assists parents in reducing and dealing with adolescents with psychosis who tend to exhibit externalizing behaviors (Kazdin, 2008; Thijssen, Vink, Muris, & de Ruiter, 2017). Understanding about illness of the patient helps the parents to deal with it more effectively. Parents are taught effective communication and problem solving styles which are helpful in gaining the trust of adolescents.
The general protocol of Parent Management Training for psychotic symptoms include the identification of early warning signs of relapse (to deal with the problem at the prodromal phase), preventive strategies (to avoid the active phase before it is too late), and techniques to deal with the active phase: (a) medicine adherence strategies, (b) communication skill training, (c) emotion regulation skills and (d) problem solving. As the patient passes the active phase, it is important to identify the common symptoms in each active phase. Parents need to be able to identify the stage and be able to decide the appropriate time to seek treatment and hospitalization of the patient with schizophrenia or schizophreniform (Agee, Spezze, & Underwood, 2014).
Sharma (2005) mentioned in the study that about thirty-nine percent of boys and twenty-three percent of girls experience their first episode before the age of 19. This is a huge percentage and if appropriate measures are taken, such as Parent Management Training, their condition may be managed without it converting in to schizophrenia.
Behavior Therapy and Parent Management Training have been recognized internationally as effective means of dealing with adolescent psychosis (Miklowitz et al., 2014; Poulton et al., 2014). There is a dearth of indigenous literature regarding the treatment and management of schizophreniform disorder especially in adolescents. More research literature is required to develop evidence based strategies to help these patients. The present study was a step towards contributing to the evidence about the efficacy of BT and PMT in the treatment of schizophreniform disorder through examining treatment outcome for a single case.
Objective of the study
The objective of the study was to assess the efficacy of Behavior Therapy and Parent Management Training in optimizing treatment outcomes for schizophreniform disorder.
Hypothesis of the study
Behavior Therapy and Parent Management Training will more likely reduce the patient‟s symptoms of anger, physical aggression (beating) towards the mother, stubbornness, use of abusive language, suspiciousness about mother, hiding things of other family members and hoarding them in his room, inappropriate association with a pet cat, poor self-care and medical non-compliance.
Method
Research Design
Single case ABA research design was used to assess the efficacy of BT and PMT for the treatment of schizophreniform disorder.
Sample
The therapy based study was conducted on 16 year old adolescent male, with symptoms of schizophreniform disorder (N=1).
Sample Characteristics/Case Description
The patient was 16 year old adolescent male, student of 10th class and was last born among four siblings. He came to Services Hospital, Lahore and was referred to Clinical Psychologist with the complaints of anger, stubbornness, using abusive language, beating mother, paranoid ideation and suspiciousness about his mother, hiding things of other family members and hoarding them in his room, not leaving the room for almost 21 hours and for about 2-3 months, inappropriate interaction with a pet cat, poor self-care, collecting his spit in a jar and medical non-compliance.
According to the patient‟s mother, his behavioral problems and symptoms started in 2005, when he was about six years old. The patient shared some of his dreams with bizarre images such as chewing a dog‟s tail. In 2005, he made suicidal threats by saying that he would jump off the roof. In 2008 also, the patient reported his suicidal ideation i.e. jumping off from the roof which remained till the age of 10. He was taking Buzon and continued with psychotherapy. From the age of 10 to 14 years, improvement was noticed in patient‟s behaviors and suicidal thoughts were not reported. The patient was taking 1/4th of the Buzon tablet and then it was stopped due to financial issues.
In 2013, at the age of 14 years i.e., three to four years after the termination of the medicines and therapy, the patient got into the company of friends who were drug addicts and involved in gambling. His mother found Naswar in his bag. She used to find cigarette boxes in his room more often. His Thin Layer Cromatography for Urine was also done and he was detoxified for the first time. After that he stopped taking the drugs as his mother kept strict notice of his whereabouts. In 2016, the patient was brought to the hospital with the presenting complaints as mentioned earlier.
In school, the patient was having extreme difficulties in the studies. Patient‟s parents were divorced and he lived with his mother. He had unhealthy relationship with his siblings.
Patient‟s maternal uncle and aunt had schizophrenia. Her maternal aunt‟s both daughters had cerebral palsy. Patient‟s eldest brother and sister had been diagnosed with Obsessive Compulsive Disorder and underwent successful treatment from the same hospital.
Written consent was taken from the patient‟s mother to voluntarily participate in the study. Confidentiality was assured. The patient was informed about the right to terminate the study at any time.
Assessment Measures
Brief Psychiatric Rating Scale (BPRS).It was administered in order to assess the positive, negative and affective symptomatology of the patient. The result showed that the patient had no somatic concerns, mild worry and depressed, and no suicidality or guilt was found. Moderate hostility towards family members, no hallucinations, elevated mood and pre-occupation about the malicious actions of other people were reported such as persecutory delusions about the mother. Unusual thought content, severe bizarre behaviors, moderate self- neglect, disorientation and conceptual disorganization, no blunted affect, emotional withdrawal, motor retardation, distractibility, mannerism, and very mild tension was observed. The results were congruent with the presenting complaints and history of present illness, and thus confirmed his diagnosis of 295.40(F20.81) Schizophreniform Disorder according to DSM-5.
Procedure
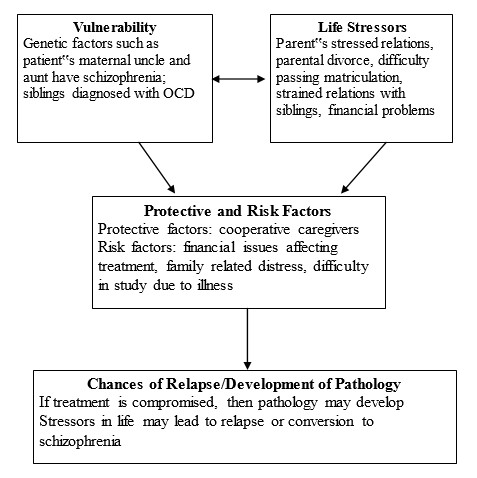
Case conceptualization.The case conceptualization of the current case was done on the basis of Stress Vulnerability Model (Zubin & Spring, 1977). Vulnerability refers to the basic susceptibility to mental health disorders. It is related to the genetic disposition and the life stressors that lead someone to become susceptible of schizophrenia.
In this case, the major vulnerability is the genetic factor which emphasizes the psychological history of family. Other vulnerability factors include financial constraints that lead to unavailability of the treatment.
Intervention
After history taking, supportive work and rapport building, the family was educated about the nature, course, prognosis and severity of symptoms. Initially, contingency contract was used with the patient to encourage him to focus on personal hygiene, keep a distance from the cat, and focus on studies. Reinforcements were provided to the patient in order to enable him follow the contract. The patient was able to follow assigned tasks. The contracts were done in subsequent sessions along with technique of Behavior Therapy i.e. Positive Reinforcement. Activity Scheduling was done to reduce the patient‟s disorganized behaviors, behaviors of isolation in a separate room, to enhance personal hygiene and enable him to prepare for exams. Anger management was done in order to deal with the aggressive outbursts of the patient with the help of techniques of BT including distraction techniques, pillow punching, and deep breathing. Later on, the patient showed compliance towards the therapy. He was taught about the stress-vulnerability model (Zubin & Spring, 1977) which led to the identification of the stressor i.e. the patient had to reappear in mathematics board exams of 9th and 10th grade. Parent Management Training was done with the mother included case conceptualization, family counseling, parenting styles, and Behavior Therapy techniques. Overall therapy was conducted in three months. After that the patient used to come for follow up sessions. The patient‟s mother was also invited to participate in the Positive Parent Management Training program seminar conducted by the therapist in the hospital which enhanced and revised the mother‟s knowledge about managing the problems of the patient and improve the communication with the patient. At the termination of therapy, blueprint was provided to both patient and his mother.
Ethical Considerations
- The patient‟s mother was told about the procedure of therapy, ABA research design, possible number of sessions, possibility of relapse, and family role. Informed consent was taken by the patient‟s mother.
- Confidentiality of the data and anonymity of the participant was maintained
- Results were reported accurately and genuinely.
Results
The therapy protocol designed for the patient after psychological assessment was consisted of Behavior Therapy and Parent Management Training. Case conceptualization helped the mother and patient to understand the causal and risk factors of the illness of the patient. Contingency contracts and activity schedule helped in eliminating odd and inappropriate behaviors of the patient. Anger management helped in managing the anger related issues of the patient. Parent Management Training also played an important part in the therapy. Mother started to follow the therapy more effectively. She realized that one of the etiological factors of the patient‟s illness is unhealthy way of communication, so PMT helped her to modify her communication style to assertive rather than being passive with the patient, she was able to deal with him in a better way.
Table 1 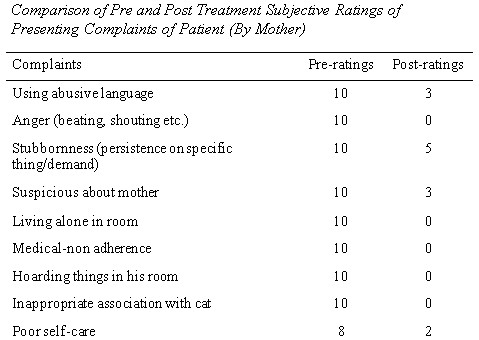
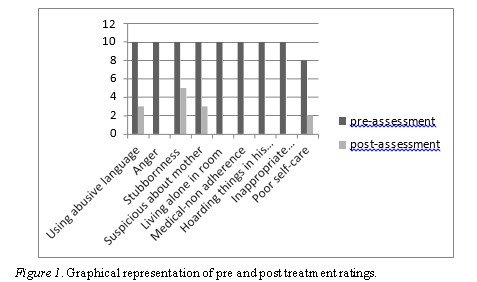
Initially, the duration of sessions with patient was less but later on increased gradually. It was done to improve the patient-therapist relationship in appropriate manner. The positive relationship led patient to follow the contingency contracts that therapist had devised in session. With the help of Positive Reinforcement technique and some other techniques form Behavior Therapy the patient was easily engaged in therapy. During Parent Management Training, the patient‟s mother was cooperative and followed the techniques at home as well. She gradually became proficient in developing contingency contracts with the patient at home. Empathy and active listening by the therapist also have aided in the therapy.
Discussion
The present study aimed to investigate the efficacy of Behavior Therapy and Parent Management Training in the treatment of schizophreniform disorder. The case was conceptualized using Stress Vulnerability Model of Zubin and Spring (1977). The result of the study revealed that the symptoms of schizophreniform can be reduced if Behavior Therapy with patient and Parent Management Training with parent are done. It proved that Behavior Therapy and Parent Management Training in treating schizophreniform is an effective treatment mode; also these findings are correlated with the literature. (Miklowitz et al., 2014; Poulton et al., 2014).
Furthermore, Behavior Therapy itself is effective in treating psychosis in adolescents. Researches show that contingency management helps a lot in dealing with the behavioral symptoms of schizophreniform (Chan, 2017; Chambless & Ollendick, 2001; Trygstad et al., 2002). Parent Management Training leads to better understanding of patient‟s illness. It gives them room to understand the parent‟s role in dealing with illness and reduce expressed emotions in the family that are directly affecting the patient (Agee, Spezze, & Underwood, 2014; Kazdin, 2008; Thijssen, Vink, Muris, & de Ruiter, 2017).
Conclusion
Patient‟s problems started in early childhood and became prominent at the age of 16. Genetic factors along with the familial factors initiated and maintained the problem. BT was applied to focus on behavioral problems and PMT was helpful in reducing the patient‟s problems with the major involvement of his mother.
Limitations and Strengths
A major role in treatment was provided by the caregivers. So the combination of Parent Management Training along with BT was a major strength in dealing with the patient‟s symptoms. The behavior techniques helped patient in dealing with his symptoms while PMT allowed the mother act as co-therapist and facilitate the improvement. Apart from this, patient‟s rapport with therapist was a source of great advantage especially when paranoia regarding the mother was dealt with in the sessions.
The limitation was the poor prognosis due to genetic and familial factors. In order to deal with this limitation, monthly follow- ups were carried out after termination of therapy.
Implications
Further research is required in Pakistan to investigate the differential effectiveness of BT and PMT in the management of schizophreniform disorder and schizophrenia spectrum disorder. Moreover, the study must be replicated in other cases of schizophrenia spectrum disorders in adolescents to find out the reliability of results.
References
Agee, E., Spezze, J., & Underwood, J. (2014). Parent Education Model for Child & Adolescent Onset Psychosis. Graduate Student Journal of Psychology, 15, 31-46.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC.
Chambless, D. L. & Ollendick, T. H. (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52(1), 685-716.
Chan, V. (2017). Schizophrenia and psychosis. Child and Adolescent Psychiatric Clinics, 26(2), 341-366.
Kazdin, A. E. (2008). Parent Management Training: Treatment for oppositional, aggressive, and antisocial behavior in children and adolescents. Oxford University Press.
Leckman, J. F. (2000). Current diagnosis & treatment in psychiatry. M. H. Ebert, P. T. Loosen, & B. Nurcombe (Eds.). Lange Medical Books/McGraw-Hill.
Liberman, R. P. & Kopelowicz, A. (1995). Basic elements in biobehavioral treatment and rehabilitation of schizophrenia. International Clinical Psychopharmacology, 9, 51-58.
Miklowitz, D. J., et al. (2014). Family-focused treatment for adolescents and young adults at high risk for psychosis: Results of a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(8), 848-858.
Perälä, J., et al. (2007). Lifetime prevalence of psychotic and bipolar I disorders in a general population. Archives of General Psychiatry, 64(1), 19-28.
Poulton, R., et al. (2014). Effects of multidimensional treatment foster care on psychotic symptoms in girls. Journal of the American Academy of Child & Adolescent Psychiatry, 53(12), 1279- 1287.
Sharma, I. (2005). Psychosis in children: What is our present state of knowledge. Journal of Indian Association for Child and Adolescent Mental Health, 1, 1-2.
Thijssen, J., Vink, G., Muris, P., & de Ruiter, C. (2017). The effectiveness of parent management training Oregon model in clinically referred children with externalizing behavior problems in the Netherlands. Child Psychiatry & Human Development, 48(1), 136-150.