Compassion Fatigue in Small Scale Health Care Facility Nurses: Testing the Effectiveness of Cognitive Behavioral Therapy
Tooba Arshad* and Kiran Bashir Ahmad
Bahria University, Karachi
The aim of the present research is to explore the levels of compassion fatigue and examine the effectiveness of cognitive behavioral therapy (CBT) on compassion fatigue in nurses working in small scale healthcare facilities. This research compares two settings i.e., Individual and Training. It was hypothesized that there would be a significant difference in the levels of compassion fatigue, before and after cognitive behavioral therapy interventions among nurses. Secondly, it was also hypothesized that there would be a significant difference in the effectiveness of cognitive behavioral therapy on compassion fatigue in nurses in individual settings, as compared to training settings. A sample of 30 nurses, recruited from two small scale healthcare facilities in Karachi were screened for compassion fatigue by using Professional Quality of Life Scale (ProQol) version 5. A total of Four nurses (M=24, SD=3.39) with high levels of compassion fatigue were facilitated by providing therapeutic intervention based on worksheets from a self-help workbook, ‘Overcoming Compassion Fatigue’ for both settings. The participants reported experiencing differing levels of compassion fatigue. Paired sample t- tests and Independent sample t- tests showed a significant difference (p < 0.05) in the levels of Compassion Fatigue post intervention. The findings also suggested absence of a significant difference (p > 0.05) in the levels of Compassion fatigue in nurses in individual settings as compared to training settings. The research carries implications for educators and psychologists as it proves the effectiveness of cognitive behavioral therapy in treating compassion fatigue. Hospital management may find it beneficial to utilize the current treatment process using cognitive behavioral therapy to relieve burnout and compassion fatigue in nurses.
Keywords: Cognitive Behavioral Therapy; Compassion Fatigue; Burn out; Secondary Traumatic Stress; Compassion Satisfaction; Nurses
Nurses engage in safe practices and provide holistic patient care which includes serving patients and giving accurate information to them and their families. Moreover, they are expected to do so while maintaining safe working conditions (Glette &Aase et al., 2017). Most nurses enter this field with the objective of helping those with critical physical, emotional, mental and spiritual needs with empathy (Lombardo & Eyre, 2011). This profession has thrived over the past century and developed into a respected and essential part of the health care. However, this still does not negate the challenges that the registered nurses face every day (Milliken & Clements et al., 2007).
Throughout the history of nursing, it is an established fact that there has been a lack of funds, personnel shortage, prolonged shifts and excessive workload as well as, an increased amount of stress while dealing with patients (Milliken & Clements et al., 2007; Johan, Sarwar & Majeed, 2017). The world appears to be short of nurses as compared to the number of patients in hospital settings, even in times of a catastrophe. Nurses are short-handed, understaffed, and overworked, often working double shifts to meet the needs when staffing is overstretched (Turley, 2005).
The Theory of Human Caring proposed by Watson (1997) puts forth relationship-based nursing (RBN) focusing on having an empathic attitude and communicating that empathy to the patients and their families (Lombardo & Eyre, 2011). Koloroutis (2007) identifies three core relationships to be transformed using RBN including their relationship with patients, self and colleagues. The core relationship most important in the management of compassion fatigue is the nurse’s relationship with herself as it is crucial for enhancing one’s health, and for being a productive member (Lombardo & Eyre, 2011).
Nurses experiencing fatigue is a common occurrence. Workload, work hours, work structures, and many other factors can indirectly or directly cause this fatigue (Dorrian & Lamond et al., 2000). Fatigue is mental or physical exhaustion that hinders a person’s ability to function normally. Nurses are expected to be ever ready for any medical emergency. This, when added to sleep deprivation and increased stress levels can lead to physical and mental fatigue. Research studies conclude that night shifts are associated with more fatigue-related outcomes as opposed to when the nurses are fully rested (Gander et al., 2018; Johnston et al., 2019). Similarly, they are emotionally worn-out as a result of accumulated stress from their work life. This combination of physical, mental and emotional fatigue can serve as factor leading to compassion fatigue. The International Council of Nurses (ICN) revealed their data about the shortage of nurses globally, and highlighted domains for action which included among others, compassion fatigue and burnout. In 2011, research conducted at Pakistan Institute of Medical Sciences (PIMS) revealed the nurse-to-patient ratio to be 1:50 (Kundi, 2011). This extreme shortage and the expectation to be ever ready in case of any medical emergency when coupled with sleep deprivation and increased stress levels, leads to fatigue. Consequently, the mental fatigue and the emotional factors provides the ideal combination for the development of compassion fatigue.
Compassion fatigue can be explained as a combination of helplessness, hopelessness, a sense of isolation and inability to be empathetic, resulting from prolonged exposure to perceived suffering (Adams et al., 2008). According to Figley, (1995) “compassion fatigue is a state experienced by those helping people in distress; it is an extreme state of tension and preoccupation with the suffering of those being helped to the degree that it is traumatizing for the helper”. Research suggests that it affects psychologists, psychiatrists, nurses, clinical social workers, emergency rescue teams, fire fighters and genetic counselors among others (Dutton & Rubinstein, 1995; Figley & Kleber, 1995). Compassion fatigue was first identified by Joinson (1992) in a study on nurses who experienced burnout while working in the emergency department. It is also known as ‘vicarious traumatization’ or ‘secondary traumatization’ (Figley, 1995).
Numerous authors have identified symptoms of compassion fatigue (Figley, 1995; Gentry & Baggerly et al., 2004; Lombardo & Eyre, 2011). The work-related symptoms consist of apprehension and therefore avoidance of working with particular patients, increased use of sick days and feeling less empathy. Post-Traumatic Stress Disorder (PTSD) has also been linked to compassion fatigue, as the symptoms are similar due to the vicarious exposure to trauma. According to the compassion fatigue awareness project, "denial is one of the most detrimental symptoms" as it hinders an individual’s ability to correctly identify the symptoms of compassion fatigue and seek help. Najjar et al. (2009) deduced that empathy is at the core of the development of compassion fatigue. Coetzee and Klopper (2009) revealed that compassion fatigue begins as compassion discomfort and progresses to compassion stress, which finally leads to compassion fatigue.
Figley and Roop (2006) characterized that compassion fatigue is a process. According to Figley’s model, it all begins when a caregiver, who is empathetic, becomes worried about a person who is suffering, leading to an empathic response by the caregiver. They are unable to distance and detach themselves from this caregiving situation, and so they began to experience dissatisfaction. This inevitably leads to compassion stress. Compassion fatigue is a result of compassion stress when the caregiver is unprotected from suffering, daunting memories and the complex demands of life (Figley, 2005). Pérez-García et al. (2021) identified the consequences of compassion fatigue from the nurses’ perspective including difficulties to carry out their work, impact on family life and the desire to quit their profession in some cases.
Compassion fatigue has been conceptualized as a multi-component construct (Zeidner et al., 2013). It comprises secondary traumatic stress, burnout and compassion satisfaction (Stamm, 2010). Burnout is related to cumulative environmental stress caused by the demands of daily life. It can be understood as a situation where the caregiver is physically and emotionally exhausted because of a decreased ability to deal with one’s environment (Medland et al., 2004).
Burnout is related to chronic over work (Kleiner & Wallace, 2017), dissatisfaction with the quality of one’s professional life, as well as departmental stress (Grigorescu et al., 2018) It emerges when goals are unachieved (Valent, 2002). A study by Bakker and Le Blank et al. (2005) revealed that burnout was contagious among nurses and younger, less experienced nurses, especially those within 2 years of graduation, are at risk of developing burnout (Rudman & Gustavsson, 2011).
Secondary Traumatic Stress, another element of compassion fatigue, is about work-related, secondary exposure to individuals who have experienced intensely traumatic and stressful events (Stamm, 2010). Numerous factors including exposure, forged bonds and empathy with patients and their families underlie nurses’ predisposition to secondary traumatic stress (Arnold, 2019). It was suggested that with the passage of time, caregiver develops some of the symptoms of PTSD - showing similar symptoms that are exhibited by the patient (Rauvola & Vega et al., 2019). Nurses who tend to injuries which are traumatic in nature or are stationed at the Intensive Care Unit (ICU) tending to critically ill patients, exhibit more increased levels of traumatic stress as compared to the nurses in general ward (Mealer et al., 2007). Additionally, nurses stationed at the emergency department (Morrison & Joy, 2016), pediatric nurses (Kellogg, 2018), and those working with suspected/confirmed COVID-19 cases (Erkin et al., 2021; Lee et al., 2021) all reported experiencing secondary traumatic stress. A study by De Figueiredo et al. (2014) on compassion fatigue and secondary traumatic stress of oncology nurses and social worker, revealed a strong positive association between compassion fatigue and secondary traumatic stress and negative association between burnout and compassion satisfaction.
Stamm (2002) introduced compassion satisfaction as the positive feeling that one experiences about their ability to help others while working in their professional fields and the extent to which they feel successful. It also incorporates the extent to which one feels supported by one’s associates. According to Dunn and Rivas (2014), for a nurse, compassion satisfaction is promoted by ongoing positive interactions and the energy experienced by them after they fulfil the needs of their patients.
Ahmed and Ali et al. (2019) conducted a cross-sectional study among nurses working at the emergency, pediatric, cardiology and intensive care units to scrutinize the manifestation of compassion fatigue, compassion satisfaction, and burnout. The results depicted average levels of compassion fatigue, compassion satisfaction and burnout which differed significantly among four clinical departments. Additionally, Khan and Khan et al. (2016), aiming to find out the association of specialty and working hours with compassion fatigue in military hospitals, revealed that working hours were associated with compassion fatigue as opposed to the speciality of field. Chances of developing compassion fatigue were significantly higher if working hours are 12 or more.
Focusing on burnout symptoms, physical demands and workload of nurses working in a small-scale facility, Zwakhalen et al. (2018) concluded that since there is less workload and hence lesser physical demands in small-scale facilities therefore, overall, there is no effect on symptoms of burnout. In another study conducted by De Rooij et al. (2012) on the mental health and burnout of professional caregivers in small scale and traditional long Term Care Settings for Elderly People with Dementia, it was deduced that emotional strain and mental health problem significantly increased with time in both types of settings with higher levels in small-scale living facilities in comparison with traditional units.
The management of compassion fatigue must be multifaceted and include prevention, assessment, and consequence minimization (Figley, 2002). Seeking professional help is only one aspect the treatment of compassion fatigue. Psychoeducation on maintaining work-life balance, and incorporating self-care plans is an effective combination for the treatment of the phenomenon. Overviewing existing literature, it has been advised repeatedly to seek professional help in order to combat Compassion Fatigue. It can help individuals to deal with the negative thoughts and stress associated with compassion fatigue (Daily Caring).
Cognitive behavioral therapy was first developed by Aaron Beck in 1960’s. The basic idea behind cognitive behavioral therapy is that the way we think (Cognitions), how we feel (Emotions) and the way we act (Behavior) are all linked together. There is evidence in favor of cognitive behavioral therapy from modern research to support its effectiveness for different psychiatric, psychological and emotional problems (Naeem et al., 2013). The main aim behind this type of therapy is to make people realize that negative interpretations impact their behavioral patterns which eventually reinforce their distorted thinking. Cognitive behavioral therapy helps people to develop alternate ways of thinking and behaving, altering their patterns which in turn change their experiences and reduce psychological distress (Martin, 2016).
According to Brunero and Cowan et al. (2008), cognitive behavioral therapy is an effective therapy for dealing with emotional distress in nurses by helping them identify cognitive distortions and challenge negative automatic thoughts. Research conducted by Motlagh and Alizadeh et al. (2014) explore the effects of cognitive behavioral therapy on nurses’ stress and conclude that cognitive behavioral techniques' significantly reduced stress. Additionally, a pilot study aiming to assess nurses’ stress levels and the effectiveness of a 1-day stress management program based on the principles of cognitive behavioral therapy, reveals statistically improved levels of overall stress as well as stress experienced at work, along with outside of work (Brunero et al., 2008).
This research is distinctive in exploring the levels of compassion fatigue and later on investigating the effectiveness of cognitive behavioral therapy on compassion fatigue in nurses working in small healthcare facilities. Pakistan is a third world country and not much attention has been given to the welfare of healthcare professionals be it in small scale or large-scale set-ups. Since nursing is a highly demanding job and the ratio of nurses and patients is unequal, the empathy exhibited by nurses for every patient leads to stress which inevitably leads to compassion fatigue. While there have been research studies on occupational stress (Khattak and Khan et al., 2011; Zehra & Faizan, 2017), little or no emphasis has been placed on exploring and treating compassion fatigue amongst healthcare professionals in Pakistan. Therefore, this study will not only fill in the wide gap in literature, but will identify and help treat compassion fatigue in nurses as well. Moreover, prior researches have analyzed the effectiveness of Mindfulness based intervention (Duarte & Gouveia, 2016), Educational Intervention (Houck, 2014) and Meditation Intervention (Hevezi, 2015). The most important goal of the present research is to facilitate the health of professional caregivers after an exposure to traumatic experiences at work through intervention and psychoeducation. This is because cognitive behavioral therapy is a solution focused therapy providing an opportunity to work at a deeper level more in-depth with the individual’s thoughts, feelings and the corresponding behaviors in the brief time of the intervention phase, it is deemed more effective therapy. This intervention-based focus on their thoughts, feelings and behavior towards themselves, others or the world in general, reduces the levels of compassion fatigue, burnout and secondary traumatic stress and increasing compassion satisfaction. .
MethodThe present research includes female nurses working at two small health care facilities in Karachi. A sample of 30 nurses (M=24, SD=3.39) from both facilities was taken and their levels of compassion fatigue were assessed by the Professional Quality of Life Scale (ProQol) version 5 (Stamm, 2010) after which four nurses with high levels of compassion fatigue, mainly, high secondary traumatic stress, high burnout and low compassion satisfaction were facilitated by providing therapeutic intervention. Additionally, this research utilizes a matched group mixed experimental design as comparisons of results of with-in group and between group were done with pre-test and post-test being conducted before and after the intervention. The sampling technique used was purposive sampling as the nurses recruited were based on the scope of the current research in which the aim was to study the levels of compassion fatigue in nurses with a certain number of years of experience along with their individual scores of the ProQol-5.
Measures Informed Consent FormThe Informed consent form briefed about the aim and methodology of the current study. The participants learned about the risk factors and benefits associated with this research. They were informed about their rights which included confidentiality and their right to leave the study at any point in time. Lastly, the nurses were asked to sign the provided contract to express their approval for the participation in this study.
The demographic information form was given to all participants to gather their basic information including their age, marital status, years of experience, number of hours working per day, how often they feel connected with their patients and the severity of patients under their supervision.
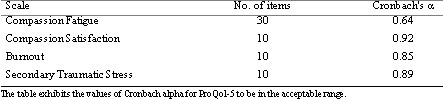
Professional Quality of Life Scale (ProQol) version 5Compassion fatigue in nurse was measured by using ProQol-5. It is a 30-item, closed ended questionnaire which could be administered either individually or in a group setting. Participants are asked to indicate their level of agreement on a five-point scale on ranges from “never” to “very often”. It is divided in to three sub-scales, that are psychometrically unique and cannot be combined with other scores. The sub-scales include: compassion satisfaction (CS) that has an alpha scale reliability of 0.86, burn out (BO), with an alpha scale reliability of 0.72 and secondary traumatic stress (STS), with an alpha scale reliability of 0.80. Good construct validity has been established of ProQol with over 200 published papers. All three scales measure separate constructs with Compassion Fatigue scale being distinct.
Procedure
Five small health care facilities in Karachi were contacted with proposals of this research to seek their willingness in order to conduct present study on nurses working there. The two facilities interested in participating were provided the official permission letter from the Institute of Professional Psychology. Researchers first ascertained the levels of compassion fatigue in a total of 30 available nurses from both the hospitals, who agreed to participate via purposive sampling. Each willing participant was given a consent form to fill in order to participate in the survey. Moreover, the demographic information form along with ProQol-5 was also given to check the levels of compassion fatigue. The nurses who scored high on ProQol-5 (mainly the ones who experienced low compassion satisfaction, high burnout and high secondary traumatic stress) and shared their willingness to participate further were facilitated by providing therapeutic intervention which comprised 7 Individual therapy sessions based on cognitive behavioral therapy. The sessions were held twice a week for 50 minutes each. Initially, three nurses scoring high on the pre-test were and recruited for therapy however, one of them backed out after the first session. Once the therapy sessions were terminated, the remaining two participants were given the post-test. A similar method was used for providing intervention in the Training (group) setting such that the training comprised of 2.5 hours. Nurses were given the consent form, the demographic information form and ProQol-5. to ascertain the level of compassion fatigue. Nurses who scored high were facilitated with a training, after which the post-test was administered.
The first small healthcare facility that was approached, gave the independence to conduct individual therapy sessions however, the second, being a nursing and midwifery school as well couldn’t allow individual sessions due to the unavailability of nurses, as they had to report to duty as well, hence a training session was conducted. The worksheets which were used and provided to the participants in both the settings were taken from a self-help workbook, Overcoming Compassion Fatigue by Teater and Ludgate (2014). The audio recording for Progressive Muscle Relaxation (PMR) is by Naeem (2014). The data collected were entered in SPSS (version 22) to run Paired Sample t-test and Individual Sample t-test.
An outline of the Session plan using Cognitive Behavioral Therapy is provided in table 1.
Table 1 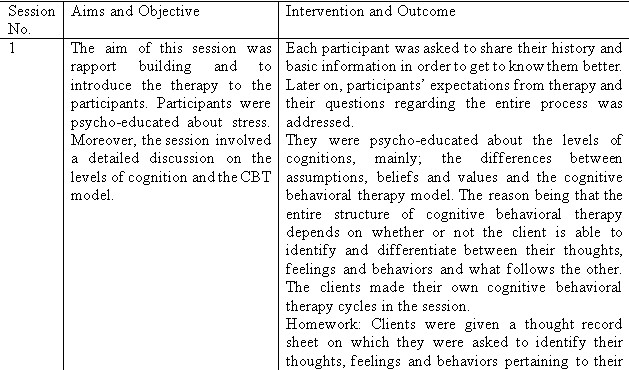
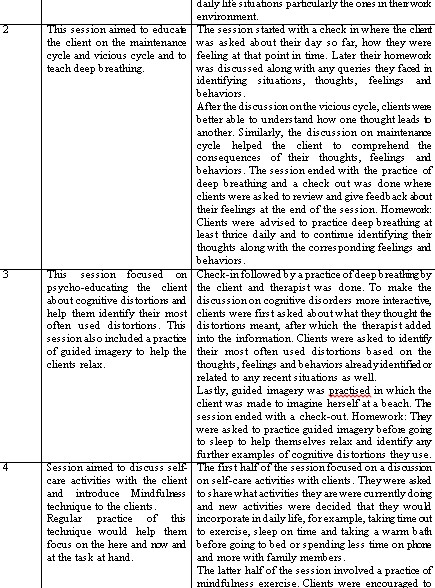
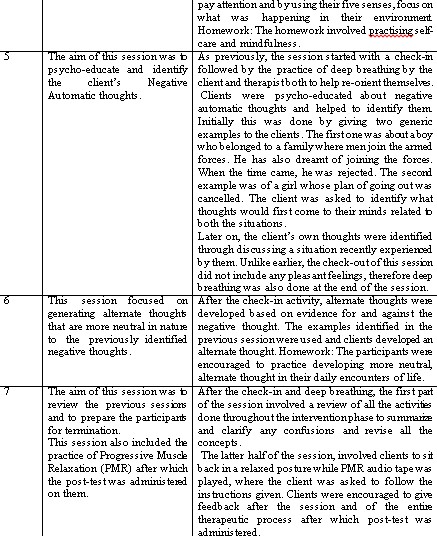
Session Plan for Training self-help workbook, Overcoming Compassion Fatigue by Teater and Ludgate (2014)
The reliability of the scale was calculated through Cronbach alpha. The difference in the pre and post-tests of variables were analyzed through paired sample t-test whereas the comparison of the difference of the two therapeutic settings i.e., individual and training sessions was conducted through the independent sample t- test.
Table 3Cronbach alpha of ProQol-5 (n=30)
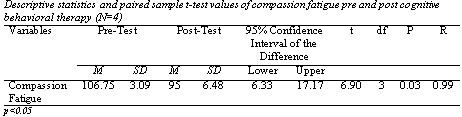
The results illustrate a significant difference (P<0.05) in the levels of compassion fatigue of the participants after cognitive behavioral therapy interventions were applied as indicated by the difference in scores in the pre and post-tests. The reduction in compassion fatigue after the intervention supports the first hypothesis i.e. there would be a significant difference in the levels of compassion fatigue before and after cognitive behavioral therapy interventions among nurses was supported (P<0.05).
Table 5 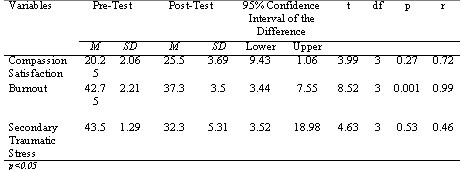
The table above illustrates the effectiveness of cognitive behavioral therapy interventions on symptoms of compassion fatigue. It is reflected through the difference in the mean values of the sub-scales of compassion fatigue of the participants after cognitive behavioral therapy was applied as indicated by the pre and post-tests. Participants initially had lower compassion satisfaction before the intervention was applied as compared to the post-test score. Similarly, they had higher burnout levels which was decreased after the intervention and had higher secondary traumatic stress before the intervention was applied as compared to the post-test scores.
Table 6 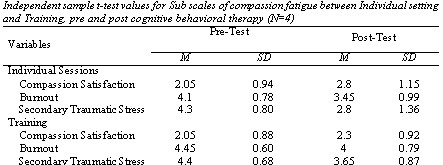
The table above illustrates the difference of effect of cognitive behavioral therapy on compassion fatigue in Individual setting as compared to Training for all sub-scales of compassion fatigue. Results indicate an absence of any significant difference (P>0.05) between individual sessions and training before and after cognitive behavioral therapy interventions as indicated by the scores of pre and post-test. However, the results do indicate a slight difference in the mean values after the interventions were applied in both the settings.
Table 7 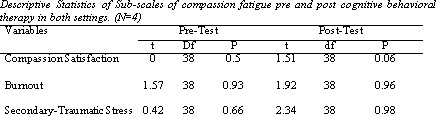
The table above illustrates that there is an absence of any significant difference in the effectiveness of cognitive behavioral therapy on compassion fatigue in nurses in individual settings, as compared to training settings from pre-test to post-test (p>0.05) therefore the second hypothesis is not supported.
Discussion
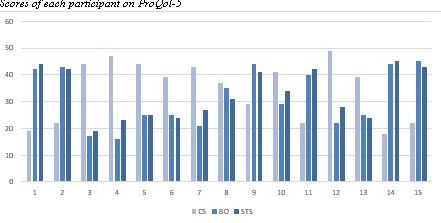
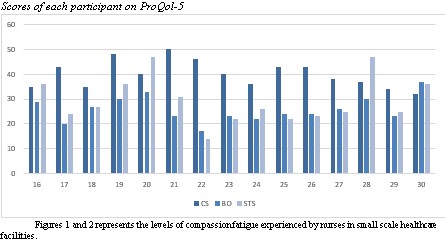
The present research was an exploratory study aimed at ascertaining whether there would be high levels of compassion fatigue in nurses working in small healthcare facilities. For this purpose, 30 nurses were recruited and their levels of compassion fatigue were ascertained. The findings indicated differing levels of compassion fatigue being experienced by nurses in this study. Later on, nurses who scored high were facilitated with sessions based on cognitive behavioral therapy. Furthermore, the present research comparatively analyzed the effectiveness of cognitive behavioral therapy on the levels of compassion fatigue in nurses in individual sessions and training through pre and post-test. The first hypothesis, which stated that there would be a significant difference in the levels of compassion fatigue before and after cognitive behavioral therapy interventions among nurses was supported as illustrated by the results recorded.
The results obtained in the present research complement the results reviewed in the literature. According to the results achieved by Motlagh and Alizadeh et al. (2014), it was found out that significant reduction in the levels of stress in nurses was observed after the intervention of cognitive behavioral therapy (p=0.03). Therefore, it was concluded that cognitive behavioral techniques' training significantly reduces stress in nurses. Similarly, the results obtained by Ohue, Moriyama and Nakaya (2015) also support the present results by concluding that CBT is an effective approach at reducing nurse’s burnout or their intention to resign based on their study.
With the application of cognitive behavioral therapy, clients were able to identify their cognitive distortions, identify and challenge their negative automatic thoughts on the basis of fact or opinion. This practice allowed them to critically evaluate their situation and bring about change in their thoughts and behaviors. Diefenbeck (2005), aiming to research whether cognitive distortions and dysfunctional attitudes in nurses plays a role in experiencing the symptoms of burnout, concluded the relationship in said variables. Additionally, when the clients identified their negative automatic thoughts, their check-out and feedback of the session revealed that they had unpleasant thoughts as compared to all the previous sessions. However, once they were able to challenge them, their feedback was much more positive. Ohue et al. (2011), concluded that by changing irrational beliefs to more rational beliefs, helping the nurses to develop positive automatic thoughts and decreasing negative automatic thoughts, the levels of burnout and stress might be prevented and nurses’ turnover can be reduced.
Focusing on the dynamics of population in the current research, it is evident that the culture of the sub-continent is such that people exhibit care and concern towards others and try to reach out to help others in need. Moreover, it is evident that people empathize with others who are in distress. Keeping the nurses’ profession in mind, it is only natural that they empathize with their patients as well. However, given the profession they are in, it can be challenging for them if they continue on doing it, inevitably leading to compassion fatigue where they are relive the trauma experienced by their patients. This is also supported by Najjar et al. (2009) who added that the basic factor in developing compassion fatigue is empathy, which is experienced by the caregiver towards their patients.
The literature reviewed and the results obtained in the present research supports that cognitive behavioral therapy is the therapy of choice to work on the nurses’ stress, compassion fatigue and PTSD symptoms as it is a short, solution- focused therapy. The focus of this therapy is on the thoughts, feelings and the corresponding behaviors as well as the consequences of those behaviors. This in turn improves an individual’s quality of life. Researches supports the view that cognitive behavioral therapy is the appropriate intervention to help individuals deal with symptoms of PTSD (Karr, 2011; Ehlers et al., 2013). Price et al. (2008), concluded that cognitive behavioral therapy is an effective therapy for reducing the symptoms of fatigue as compared to other therapies. Babineau et al. (2019), further added that cognitive behavioral therapy can help is reducing symptoms of burnout in individuals.
The second hypothesis of the present research stated that there would be a significant difference in the effectiveness of cognitive behavioral therapy on compassion fatigue in nurses in individual settings as compared to training settings. The results illustrated an absence of any significant difference; therefore, the second hypothesis was not supported.
Shifting our attention to the dynamics of the population in the current research, an important factor to keep in mind is that therapeutic interventions were being provided at their work place therefore some degree of resistance from the participants was expected. Even with the current trend of creating awareness for mental health issues in Pakistan, not many people are comfortable in visiting a psychologist to discuss any issue in their lives. The acceptance, though, has increased as compared to before, but it is still considered taboo to visit a professional to seek help related to mental health issues. A thought shared by one of the participants helped the researchers understand their view as this feeling of resistance would have been increased when the colleagues would comment and ask about the happenings of each session particularly about why they were attending sessions in the first place.
Moreover, even with all the reassurance, participants might have doubts and believe been that the things discussed during sessions would be communicated to the higher officials of the hospital, therefore creating problems in their workplace or create a threat for their future in that hospital. All of the aforementioned reasons might have contributed to why a participant chose not to continue participation in the present study after taking the first session.
A common observation by the researcher was that even during the sessions, the participant would be called to attend to a patient thus, creating a hinderance in the flow of therapy sessions. The participants would often feel obliged to leave mid-way, as part of their responsibility and empathy towards their patients. This personal factor of empathizing with their patients could have contributed to the results recorded.
ConclusionThe current study provides evidence that due to the nature of their work, nurses of small-scale health care facilities of Karachi experience compassion fatigue. Additionally, cognitive behavioral therapy has been proving to be an effective therapy for compassion fatigue in nurses. It is important that hospital management play their role in facilitating nurses experiencing compassion fatigue by providing them with avenues to seek help.
ImplicationsThe present study can benefit educators and psychologists as it proves the effectiveness of cognitive behavioral therapy in treating compassion fatigue. Moreover, it has great implications for the nurses’ population as this study not only validates their concern, but also reassures that it can be effectively dealt with. Additionally, this research can help psychologists by providing a framework for any future intervention-based studies in Pakistan as it compares two therapeutic settings i.e., Individual and Training. Hospital management may find it beneficial to utilize the current treatment process using cognitive behavioral therapy to relieve burnout and compassion fatigue in nurses.
Limitations and RecommendationsApproaching the healthcare facilities that were allowing their nurses to take part in this study has been the greatest challenge. As a result of this, the biggest limitation is that the sample size is very small. Therefore, it is recommended that psychologists work in groups to approach healthcare facilities for interventions. Moreover, since the sample size is very small, particularly the training group, there is greater chance that extraneous variables might be present, which would have impacted the study and made the training less effective. Another limitation is that a follow up session couldn’t be scheduled. Additionally, the session plan mostly included the cognitive element of therapy. If equal emphasis had been given to behavioral experimentation, the participants would have had a chance to actually apply what they have learned in the intervention phase, and could have received an on-ground experience which would have had great impact on the results of the study. Lastly, the frequent calling to duty for the participants during their session created a hindrance in the flow of therapy.
Due to the small sample size, the results proved to be insignificant however, this justifies the need for further research to be done in this area. It is also recommended that if group trainings are being provided to nurses, then they should comprise of a greater number of sessions in order to make the process more thorough. This is recommended because nurses might not be available for one-to-one sessions for longer periods of time due to their professional constraints, and because more nurses could be catered to this way. Additionally, future studies can compare or can focus on male nurses, which can lead to interesting findings. Lastly, it is recommended that while such interventions are provided to nurses, hospital management should improve their scheduling so a more lasting impact can be achieved by the participants. However, this was not the scope of the current study, but may be done in future.
ReferencesAdams, R.E., Figley, C.R., Boscarino, J.A., (2008). The Compassion Fatigue Scale: Its use with social workers following urban disaster. Research on Social Work Practice, 18 (3), 238–250. https://doi.org/10.1177/1049731507310190
Ahmed, T., Ali, A., Rasheed, A., & Naz, S. (2019). Compassion satisfaction, compassion fatigue and burnout among nurses working in clinical departments at a tertiary care hospital in Karachi. Pakistan Journal of Physiology, 15(3),19-22. .http://www.pjp.pps.org.pk/index.php/PJP/article/view/1084.
Arnold, T. C. (2020). An evolutionary concept analysis of secondary traumatic stress in nurses. Nursing Forum. 55, 149– 156. https://doi.org/10.1111/nuf.12409
Bakker, A.B., Le Blanc, P.M., & Schaufeli, W.B. (2005). Burnout contagion among intensive care nurses. Journal of Advance Nursing. 51(3),276-87. https://doi.org/10.1111/j.1365-2648.2005.03494.x
Babineau, T., Thomas, A. & Wu, V. Physician Burnout and Compassion Fatigue: Individual and Institutional Response to an Emerging Crisis. Current Treatment Options in Pediatrics 5, 1–10 (2019). https://doi.org/10.1007/s40746-019-00146-7
Brunero, S., Cowan, D., & Fairbrother, G. (2008). Reducing emotional distress in nurses using cognitive behavioral therapy: A preliminary program evaluation. Japan Journal of Nursing Science. 5(2),109-115. https://doi.org/10.1111/j.1742-7924.2008.00102.x
Coetzee, S.K., Klopper, H.C. (2010). Compassion fatigue within nursing practice: a concept analysis. Nursing and Health Sciences. 12(2),235-43. https://doi.org/10.1111/j.1442-2018.2010.00526.x
Craig, C.D., & Sprang, G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress & Coping: An International Journal. 23, 319-339. https://doi.org/10.1080/10615800903085818
De Figueiredo, S., Yetwin, A., Sherer, S., Radzik, M., & Iverson, E. (2014). A cross-disciplinary comparison of perceptions of compassion fatigue and satisfaction among service providers of highly traumatized children and adolescents. Traumatology, 20(4), 286–295. https://doi.org/10.1037/h0099833
De Rooij, A. H., Luijkx, K. G., Declercq, A. G., Emmerink, P. M., & Schols, J. M. (2012). Professional caregivers’ mental health problems and burnout in small-scale and traditional long term care settings for elderly people with dementia in the Netherlands and Belgium. Journal of the American Medical Directors Association, 13(5), 486-e7.