Overview and Treatment of Perceptual Distortions in Patient of Schizophrenia: A Clinical Case Study
*Hajra Fareed
University of the Punjab, Lahore, Pakistan
Hira Fatima
Lahore General Hospital, Lahore, Pakistan
The case highlights the management of Schizophrenia in a 35 year old married woman. In this case, assessment of the client was done informally through Baseline Charts, DSM-5 checklist, and Mental Status Examination while for formal assessment, Brief Psychiatric Rating Scale (BPRS) and Symptom Checklist-R was administered. Considering the scores and complaints, client was diagnosed with 295.90 (F20.9) Schizophrenia with first episodes currently in the acute phase. Seventeen sessions were carried out with 45-60 minutes for each session. Techniques of Cognitive Behavior Therapy were found to be an effective improvement in the client’s hallucinations which can be seen through reduced frequency on baseline chart and hallucinatory behavior in the BPRS scale. The family was psychoeducated. It was concluded that CBT is effective in managing the symptoms of Schizophrenia.
Keywords: Schizophrenia, perceptual distortions, cognitive behavior therapy
Schizophrenia is a severe mental disorder. It is characterized by distortions in thinking, perception, emotions, language, sense of self, and behavior. It affects 0.3% to 0.7% of adults worldwide. It can occur between the ages of 5 to 60 years with earlier onset more in males and later onset in females. The chance of having schizophrenia is more in individuals from the urban area in comparison to rural areas (Jones, 2013). According to DSM-5 (APA, 2013), it is characterized by delusions, hallucinations, disorganized speech, catatonic behaviors, and negative symptoms. The symptoms cause disturbance for at least 6 months. Hallucinations and delusions can pose a threat in terms of altering a person’s connection with themselves and the world around them. This threat can be attributed to the disruptions in perceptual processing seen especially as a marker for the onset of schizophrenia highlighting an important target for further research and pathophysiology of schizophrenia (Ulhas & Mishara, 2007).
One of the prevalent symptoms of schizophrenia is hallucination or else known as perceptual distortions. Perception is defined as the disambiguate interpretation of the sensory inputs from the environment. As it is related to the sensory system, it is clear that the perception of patients having schizophrenia becomes false in various sensory modalities such as auditory, visual, tactile, olfactory, or gustatory; with auditory being the most rampant. It has been reported that hallucinations, unlike other symptoms of schizophrenia, are distinguishable and are diagnosed using informal and formal assessments. After assessment, their symptoms can be addressed through medication and therapeutic intervention (Waters & Frenehough, 2017).
Objective of the Study
The objective of the study was to evaluate the efficacy of Cognitive Behavior Therapy for treating perceptual distortions.
Hypotheses of the Study
Cognitive behavior therapy will significantly reduce the client’s complaints regarding auditory and visual hallucinations (perceptual distortions) Furthermore, CBT will reduce delusional beliefs, sleep problems along with aggression and irritability.
Method
Research Design
Single case ABA research design was used to assess the efficacy of cognitive behavior therapy in dealing with disturbed perceptual differences.
Sample Characteristics/ Case description
S.R., a 35-year-old married woman, belonged to a lower socio-economic class. She was initially attended at the OPD (outdoor psychiatric patient ward) at a government hospital in Lahore in an emergency. Upon assessing her condition, she had been referred to the psychiatry ward for further evaluation of her symptoms and treatment accordingly.
Background Information. The client was born on 20th March, 1983 in Lahore. She was the eldest among her 4 siblings (3 sisters and 1 brother). The client started school at the age of 4 years. She was not fond of studying but enjoyed spending time with her friends. She had a friendly relationship with her teachers. The client completed her education till intermediate. The personal history of the client revealed that there were no perinatal and post-natal complications. The client had a healthy childhood. As reported, S.R. had no problems during the menstrual phase as she had an insight about the period cycle and it was further explained well to her by her mother. As reported by the client’s sister, being the eldest daughter, was extremely attached to their father as she would spend most of her time with him and share all her feelings, thoughts, and problems with him. The client was dearly loved by both parents as she had a sensitive nature. Her sister reported that she would get stressed and upset on trivial matters for which the parents would ensure to keep her happy. The client's sister reported that S.R. had a congenial relationship with all siblings and showed a sense of responsibility towards them especially with the youngest one. The premorbid personality of the client revealed that she was a fun-loving, energetic, warm, and caring young woman who thoroughly enjoyed the pleasant moments of life. Her sister reported her to be fond of nature and showed interest in household chores like cooking. However, the client became serious in 2002 when she lost her father. She remained disturbed for a long time and was reported to become quiet and more serious. She had not yet recovered from the grief of her father's death when her mother passed away a year later. The client was devastated however the clients' brother gave her ultimate support and care which helped her in overcoming the sorrows.
S.R. got married at the age of 20 years to her cousin who did not treat her well from the beginning with strong interference from her mother-in-law and intrigues to set S.R. up, leading to S.R. and her husband having frequent quarrels and acts of domestic violence perpetrated towards her. S.R. had three children with her husband (she had three boys the eldest one aged 14 years, the middle one of 11, and the youngest to be of 5 years at the time of treatment). It was reported that despite living for 17 years into a marriage and serving her in-laws and husband with complete devotion, the environment was never favorable for S.R. She continuously had to face domestic abuse. She would mostly remain fearful and stressed of what actions of hers will be misunderstood by her mother in law and told her husband with a lot of manipulation resulting in a quarrel and often physical abuse. As the client loved her husband dearly, she tolerated and justified his behaviors. However, incessant violence affected the client’s health. In 2016, she was diagnosed with a brain tumor. She was treated for a brain tumor for around 6 years initially with medication and then they had to go for surgery in August 2017. After the surgery, the client remained on a ventilator for one day and survived. During this period, S.R.’s husband took no financial or moral responsibility rather the client's brother had to support her.
Once the client got healthier from the ailment, she went back to her in-laws. The client's husband showed care for her for no less than a few months till his sister (married to the client’s brother) took divorce in August 2017. The in-laws pressurized their son to divorce the client. The client reacted to it, with an extreme anger outburst, to which the inlaws forcefully admitted her in the mental hospital of Lahore. She stayed there for 8 days and was taken out by her siblings after they came to know about it. The client was brought to her parents’ house by her brother. She stayed there for 3 months in which she tried several times to contact her husband but he never responded to her calls.
In February 2018, the client's husband sent the first divorce followed by 2nd and 3rd. During the entire period, client was unable to have a contact with her husband to which she was extremely dismayed. She tried to call her husband for her children but they did not allow her to meet. The client was baffled. She was given hope by her brother who, in December, 2018, passed away in an accident. It hit the client like a rock. She was not able to accept that her brother was no more. The client’s sister reported that she was often seen at night, talking to herself and smiling and when asked would say it is our brother and sometimes seen putting hands on her ears and shouting at someone that you are lying. She remained extremely irritable.
In April 2019, she was brought to the hospital with complaints of aggressive outbursts, self-talking, self-laughing, delusions, hallucinations, reduced appetite, and sleep. Her organicity was ruled out. She was referred to a trainee clinical psychologist for the assessment and management of her symptoms.
No history of psychiatric illness in the family was reported. Ethical considerations were fulfilled such that confidentiality was ensured and informed consent was taken from the attendant.
Assessment Measures
Mini-Mental Status Examination
The client was a 35-year-old Muslim woman of tall height and average weight. She was dressed in mismatched clothes such that she was wearing a different colored shalwar (trouser), kameez (shirt), and dupatta (a large scarf covering her shoulder and head); the mood was irritable and she was non-cooperative towards the interviewer. She was loud and would start to look out of the window talking and smiling at someone stating her children are here. The client had no obsessions yet delusions were observed along with visual and auditory hallucinations were present. Suicidal ideation was not observed. The client had poor time orientation, judgment, attention concentration, abstract thinking, and lacked insight about her illness. Scores on mini-mental status examination showed cognitive impairment.
Baseline Charts
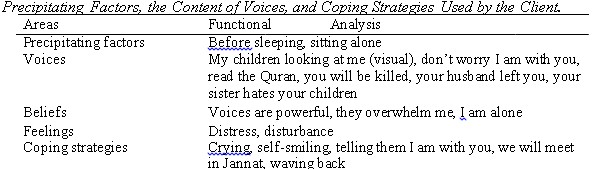
Baselines were taken for the voices that she heard to determine the frequency and intensity of the voices that she heard along with the precipitating factors, the content of voices, feelings, and coping strategies.
Table 1
Brief Psychiatric Rating Scale (Overall & Gorham, 1962)
On the Pre-Assessment level, Brief Psychiatric Rating Scale (BPRS) was administered before applying the treatment plan to check the symptoms of schizophrenia. The total score on BPRS is 83. The score indicates an individual to be severally ill as the cutoff between 70 to 85 indicates the baseline for the severity of schizophrenia. Similarly, a high score on suspiciousness, hallucinatory behaviors, uncooperativeness, unusual thought content, and disorientation indicating symptoms of schizophrenia (see table 2)
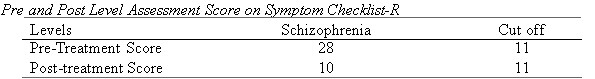
Symptom Checklist (Rahman et al., 2009)
The qualitative interpretation of the sub-scale of schizophrenia on Symptom Checklist-R showed that the score, 28 is above cut-off (17) assuring the diagnosis of schizophrenia (See table 3 for pre and post-assessment)
Based on the formal and informal assessment the diagnosis of S.R. was given the diagnosis of 295.90 (F20.9) Schizophrenia, first episode in acute phase.
Procedure
Case formulation
The client was a 35-year-old woman showing symptoms of visual and auditory hallucination, paranoid delusion, aggressive outbursts, restlessness, irritability, and poor appetite and sleep. The case was formulated based on relating the theories with the client’s history. The following formulation was based on
According to the psychodynamic perspective, schizophrenia develops from two psychological processes i.e. regression to a pre-ego stage and efforts to reestablish ego control. Freud proposed that when their world has been extremely harsh or withholding—for example, when their parents have been cold or non-nurturing or when they have experienced severe traumas—some people regress to the earliest point in their development, to the pre-ego stage of primary narcissism, in which they recognize and meet only their own needs. This sets the stage for schizophrenia (Bebbington, 2018). The following perspective relates to the theory in such a way that the client had experienced an extremely harsh time after her marriage whereas the time before her marriage had been pleasant. She is the eldest and dearest to her father had lived life as an authority but after marriage leading to divorce and the death of parents and brother lead her regress to the past life.
According to the cognitive explanation, when people attempt to understand their unusual experiences, more psychotic features emerge (Comer, 2013). When first confronted by voices or other troubling sensations, these people turn to relatives and friends. Naturally, when relatives and friends deny the reality of the sensations, eventually the sufferers conclude that others are trying to hide the truth. They reject all feedback and develop beliefs (delusions) that they are being persecuted. This concept is known as the theory of mind (Beck & Rector, 2003). The cognitive perspective relates to the client such that the understanding of divorce and having to let go of her children lead to a troubling sensation that is forming delusions. She believed that her sister is the one plotting against her, deceiving her and disliking her.
Environmental stressors play an essential role in causing schizophrenia. Contracting the disease leads to social and economic downward drift i.e. one sees a downfall in social and economic life due to the disease or the disease causes a social and economic drift. The client experience hostile behavior from the in-laws and husband. The death of her brother and divorce were great stressors making her vulnerable towards the disease.
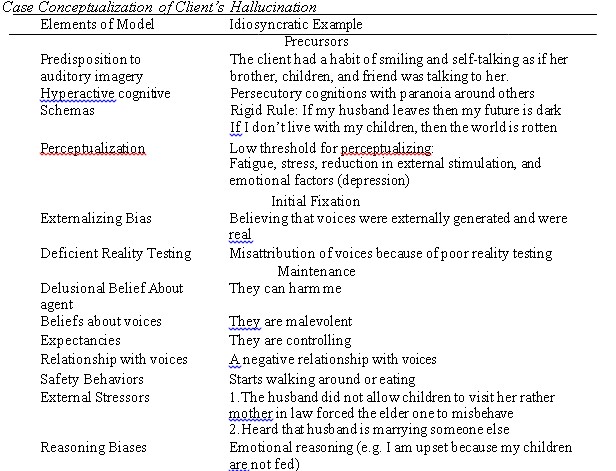
Case Conceptualization of Hallucination (Beck & Rector, 2003)
The present case was conceptualized according to the model of hallucination by beck and rector as shown in table 2.
Table 2
Intervention
After a thorough assessment and formulation of the client treatment plan were implied based on techniques of cognitive-behavioral therapy. In the initial sessions, focus was to build a therapeutic alliance with the client to enhance the efficacy of therapy. The client was given the understanding that she is being understood and shall be given unconditional positive regard. Confidentiality was obtained along with psychoeducation of the client and the family on dealing with symptoms of schizophrenia. Rapport building played an essential role in proceeding with the therapy plan. The next session was followed by psycho-education and normalization. The client was told that when distressed or emotionally upset one can hear voices and there is part of schizophrenia. The family was emphasized for keeping a check for medication adherence and the client herself was ensured about it. The following activities were carried out in sessions 1-3.
In session 4-7, the client was socialized to the conceptualization model along with the understanding that how events, thoughts, and feelings are connected and have an influence on one another. It was difficult for the client to understand initially therefore, a simple example of daily life was taken to explain it. It was followed by behavioral work for hallucinations which include coping statements (e.g. I am strong enough to try) and distraction techniques for auditory hallucinations (e.g. putting earplugs, listening to audios in the loud sound of their choices, walk, etc.). Any technique that helped the client to distract herself along with reducing the anxiousness caused by voices were applied (e.g. watching tv, making conversation) along with relaxation exercises. Similarly, if the client found it still distressing, she was asked to remove herself from the place where she was hearing those voices.
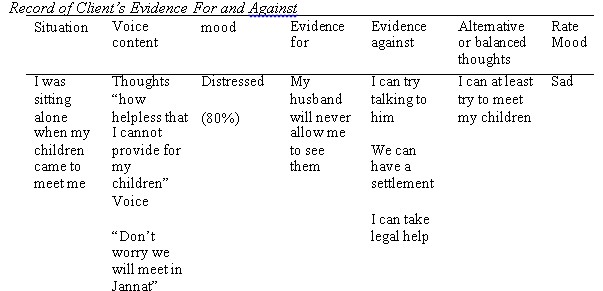
From the 7th session onwards cognitive work was done with the client by targeting her voice content using peripheral questioning. As the voice content becomes grounds for delusional beliefs, it is a series of questions about the person’s belief system to understand how the patient arrived at his conviction (Turkington & Siddle, 1998). Peripheral questioning was done with the client to shake her belief along with Evidence for and against was applied in which the client is asked to evaluate what evidence there is in favor of the behavior and what is against. It helps in analyzing whether the behavior is logical or illogical (Leahy, 2003). The client's perception was shaken after she stated the evidence for and against her beliefs as shown below in table 3. The table shows a sample of clients’ beliefs against her voices questioned using evidence for and against.
Table 3
Further, with the same belief, a concept of psychoanalytical theory i.e. reality testing was applied in which the ego recognizes the difference between the external and internal world. It is the ability to see a situation for what it is rather than what one fears or beliefs. The rationale is to make the client get intact with reality (Chadwick et al., 1996). In reality testing, the client was asked to observe and see whether the voice she hears of her children or when she sees them, are they seen by others around. Other members of the family were also asked about it. After experimenting, it was initially distressing for the client but it gradually began to reduce its conviction. The conviction required practice until the last session. Similarly, the techniques were applied with the client’s delusions and it worked for hand in hand in reducing both. As the client had reported improvement in her symptoms and it was observable thus from session 12-15 self-management, stress vulnerability model, problemsolving, vocational training, and assertiveness training were explained to reduce the chances of relapse and help the client function well. The techniques were explained one by one in detail and then carried out in session with the client where initially she was given a hypothetical example and then asked to place in one of her examples to ensure that she understood these techniques well. The techniques were found to be effective with the client.
In session 15-17, therapy blueprint was given and follow up sessions were conducted.
Results
After the management of the client’s complaints, post-assessment was done. The results of the post-assessment are provided in the tables below.
Table 4
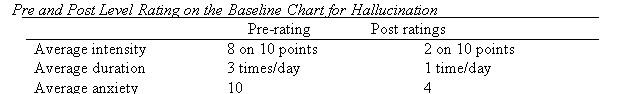
Table 5
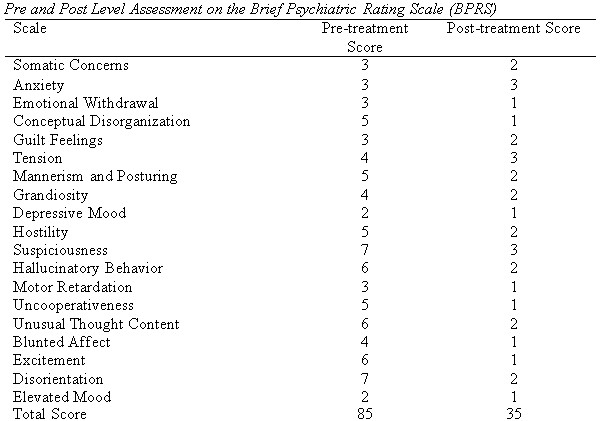
Figure 1
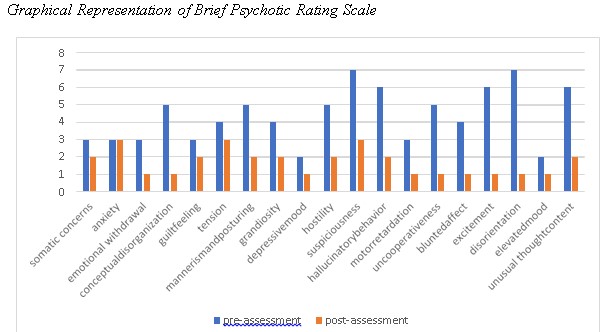
Table 6
Discussion
The client in the present case displayed auditory and visual hallucinations as a symptom of schizophrenia due to the stressor of divorce, not able to meet her children, and the death of her brother. The client remained restless, showed mood incongruency, delusions, disorganized speech, appetite reduced as well as sleep, and remained pre-occupied with the concern for her children. The following symptoms were consistent with the Schizophrenia diagnosis according to DSM-5. According to DSM-5 (APA, 2013), an individual experiencing 2 out of 5 of the following including hallucination, delusions, disorganized speech, catatonia for most of the time for at least 6 months and causing significant clinical distress in daily functioning indicates the diagnosis. The symptoms helped in formulating the diagnosis of the current client.
The present study aimed at investigating the efficacy of cognitive-behavioral therapy in dealing with hallucinations along with co-occurring symptoms in clients with schizophrenia. The results of the study showed the effectiveness of cognitive behavior therapy in the management of the symptoms. The study is consistent with the previous literature. As stated by Pfammatteret al. (2006) carried out a meta-analysis on the efficacy of psychological therapies in Schizophrenia. The findings from randomized controlled trials and meta-analysis suggested that social skill training, cognitive remediations, psychoeducation, coping intervention, family therapy, and cognitive behavioral therapy resulted in the reduction of positive symptoms.
Similarly, according to Beck and Rector (2003) peripheral questioning has been linked with graded reality testing to reduce the impact of positive symptoms. They were
carried out to postulate that clients' doubts and speculations. The techniques were found to be helpful by the therapist in unblocking the conviction that the client had in his beliefs and reduce the distress evoked by the delusions. Similarly, Dannahy et al (2011) examined the impact of the group-based cognitive therapy for distressing voices. A sample of 62 was taken as participants and 8-12 sessions were conducted. The pre and post assessment showed significant improvement.
Conclusion
With the help of techniques, the client had overcome her symptoms of perceptual distortion along with co-occurring symptoms. The limitations of the therapy were that the stressor from her ex-husband was present. The stressor of not meeting her children was troubling. Thus, more work could have been done regarding the emotional processing of the client.
References
American Psychological Association. (2013). Diagnostic and statistical manual for mental disorders (5th ed.). http://doi.org/10.1176/appi.books.9780890425596
Bebbington, P. E. (2018). Sexual abuse and psychosis: the security of research findings. Schizophrenia research, 201, 37-38.
Beck, A. T., & Rector, N. A. (2003). A cognitive model of hallucinations. Cognitive Therapy and Research, 27, 19–52.
Chadwick, P., Birchwood, M.J., & Trower, P. (1996). Cognitive therapy for delusions, voices and paranoia. Wiley
Comer, R.J. (2013). Fundamentals of Abnormal Psychology. Worth Publishers.
Dannahy L, Hayward M, Strauss C, Turton W, Harding E. & Chadwick P. (2017). Group person- based cognitive therapy for distressing voices: Pilot data from nine groups. Journal of Behavioral Therapy Experiment in Psychiatry, 42, 111–116.
Jones, P. B. (2013). Adult mental health disorders and their age at onset. The British Journal of Psychiatry, 54(1), 5-10.
Leahy, R. (2003). Cognitive therapy techniques: A practitioner’s guide. The Guilford Press.
Overall, E.J. & Gorham, D.R. (1962). Brief Psychiatric Rating Scale. Psychological Reports, 10(3), 799-812.
Pfammatter, M., Junghan, U. M., & Brenner, H. D. (2006). Efficacy of psychological therapy in schizophrenia: conclusions from meta-analyses. Schizophrenia bulletin, 32(1), 64– 80. https://doi.org/10.1093/schbul/sbl030.
Rahman, N. K., Dawood, S., Rehman, N., Mansoor, W., & Ali, S. (2009). Standardization of Symptom Checklist-R on a psychiatric and non-psychiatric sample of Lahore city. Pakistan Journal of Clinical Psychology, 8, 21-32
Turkington, D & Siddle, R. (1998). Cognitive therapy for the treatment of delusions. Advances in Psychiatry Treatment, 4(13), 235–242